Skin lesions and blemishes are very common. Most of them are benign and have no malignant potential. But some can be malignant or potentially malignant. Some areas of the body are easy to examine but other parts of the body are not clearly visible. One such area is lower part of a woman’s breast.
Many women are very particular in doing breast self-examination but forget to do visual inspection of the nipples, areola and under surface of the breasts where moles can be missed.
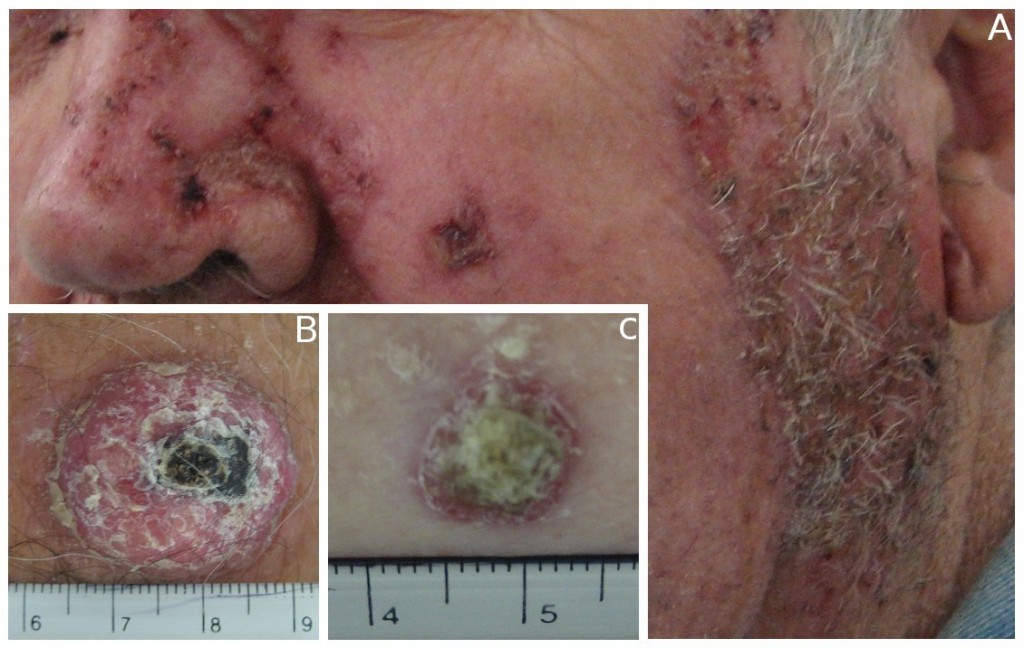
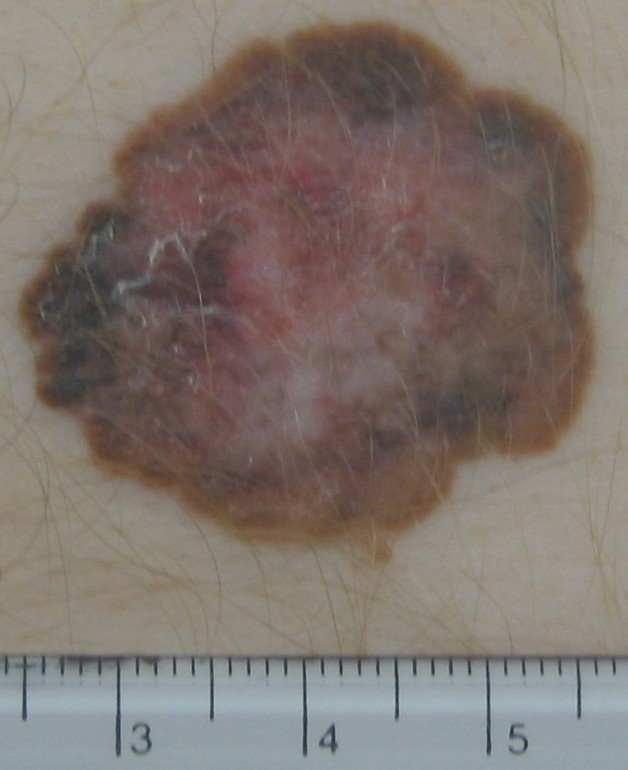
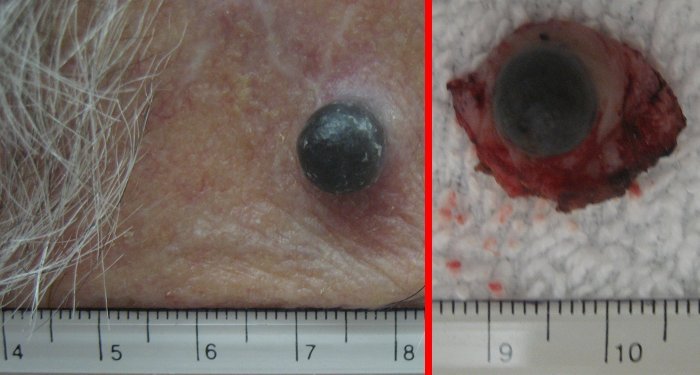
Moles that are of medical concern are those that look different than other existing moles or those that first appear after age 20. If you notice changes in a mole’s colour, height, size or shape, you should have these moles checked. If the moles bleed, ooze, itch, appear scaly or become tender or painful then it is time to have them removed and checked for cancer.
The following ABCDEs are important signs of moles that could be cancerous:
Asymmetry – one half of the mole does not match the other half.
Border – the border or edges of the mole are ragged, blurred or irregular.
Colour – the colour of the mole is not the same throughout or has shades of tan, brown, black, blue, white or red.
Diameter – the diameter of a mole is six millimetres or larger.
Evolution – moles which have changed over a period of time.
Remember, there is a forecast for a sizzling summer this year. So, we should continue to remind ourselves to protect the rest of the body from sunburn. Use of sunscreen is one way to do it. There is a lot of misconception about what kind of sunscreen to use and how to apply.
Sun Protection Factor (SPF) 30 provides 30 times greater sun protection than unprotected skin when exposed to damaging sun’s ultraviolet B (UVB) rays. This does not mean you can stay in the sun for 30 hours without burning yourself. Sunscreen should be applied liberally and often depending on how much you sweat and how wet you are. Make sure the sunscreen blocks UVB and UVA. Higher SPF provides better protection. Wear protective clothings, wide brimmed hat, sunglasses which block both ultraviolet rays.
The best protection against sun’s damaging rays is to stay away from the sun and take your vitamin D regularly. I guess that is too much to ask, especially when our summers are so short. So enjoy the sun but be sun smart.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!