“The wearing of face masks during the 2019 – 20 coronavirus pandemic has received varying recommendations from different public health agencies and governments,” says an article in Wikipedia.
An editorial in the British Medical Journal (COVID -19: should the public wear face masks? – BMJ 09 April 2020) says, “Yes – population benefits are plausible and harms unlikely.”
Is there any direct evidence that wearing a mask would help? The editorial concludes, “…given the gravity of the pandemic, indirect evidence of benefit combined with the low risk of harm should outweigh the absence of direct evidence supporting mask wearing by the general public.”
It has been about five months since COVID-19 hit the headlines and spread infection all over the world. Since then one of the big topics of discussion has been “to wear or not to wear” a face mask. There has been so much disagreement and debate among health agencies and governments, it has left the public confused.
Some groups recommend that all members of the public wear masks, while others recommend that only COVID-19 patients and their caretakers should wear them.
In some countries it is mandatory to wear a face mask. On the other hand, other countries are still struggling to provide appropriate advice to the general public. To top it all there is an acute shortage of masks.
Types of face masks, from least to most protective, include:
- Cloth face masks: Although good quality evidence is lacking, some data suggest that cloth masks may be only marginally (15 per cent) less effective than surgical masks in blocking emission of particles, and fivefold more effective than not wearing masks. Therefore, cloth masks are likely to be better than wearing no mask at all (BMJ).
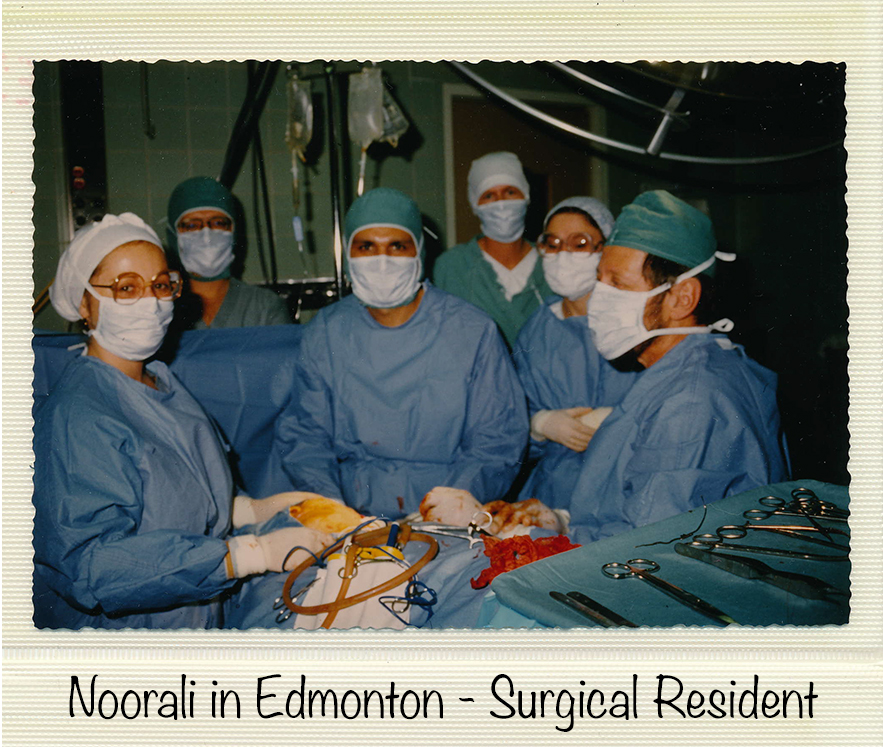
- Surgical masks: The standard surgical mask, also known as a fluid-resistant surgical mask (FRSM) is designed to provide a barrier to splashes and droplets for wearer of the mask. It fits fairly loosely to the user’s face. They are used for a variety of procedures in community as well as hospital settings. These are single-use masks. They should not be undone and dangled round the neck between procedures. It should be worn with eye protection.
Surgical masks do not provide complete protection from germs and other contaminants because of the loose fit between the surface of the face mask and the face. Surgical masks may be labeled as surgical, isolation, dental, or medical procedure masks.
Surgical masks are recommended for those who may be infected, as wearing a mask can limit the volume and travel distance of droplets dispersed when talking, sneezing, and coughing. - N95 masks: Also known as respiratory mask. It is a disposable mask. Masks ending in a 95, have a 95 per cent efficiency. An N95 mask is a particulate-filtering facepiece respirator. It filters at least 95 per cent of airborne particles. It is the most common respirator used in health care.
- Face shields and medical goggles are other types of protective equipment often used together with face masks.
In summary, personal protective equipment, including devices such as N95 respirators, gowns, masks, gloves and face shields, are medical devices in Canada and are subject to requirements under the Medical Devices Regulations. They should be used appropriately. Hope the information provided here helps. Be safe. Stay healthy.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!