In September, 2002 a mosquito bit a Toronto resident, George Eliopoulos. He subsequently died due to West Nile virus. Eliopoulos was in his 60s. His family is now suing the Ontario government alleging it failed to properly implement its 2001 West Nile virus surveillance and prevention plan.
The case is slowly going through the judicial system. Bill Rogers, legal columnist for the Medical Post says the Ontario government has lost two written judicial pronouncements. But the case is far from over. The court has still to decide whether this case can go to court.
There are 40 other individuals who contracted West Nile virus in 2002 are also suing the Ontario government.
The law suits claim that the government of Ontarios May 2001 plan for surveillance and prevention of West Nile virus was deficient and the government failed to implement it in a reasonable and careful manner.
One of the issues the court has to decide is whether Ontario governments West Nile virus plan was a government policy. If so, then governments cannot be sued for their policy, says Rogers. The court will also decide if government negligence caused deaths due to West Nile virus.
*********************************************
A report in the Canadian Medical Association Journal (CMAJ) says doctor shortage is increasing in Canada. The proportion of family physicians accepting new patients declined from 23.7 per cent in 2001 to 20.2 per cent in 2004. This shortage is going to get worse as 3800 physicians plan to retire this year.
Currently, 24 per cent of Canadas doctors are international medical graduates. In Saskatchewan, more than 50 per cent of doctors are international medical graduates.
Part of the problem, says CMAJ report, is that there are only 6.5 medical school positions per 100,000 population in Canada compared to 12.2 openings in the U.K. The second problem is lack of sufficient residency programs. If medical school positions are increased then the residency programs will have to be expanded. When is this going to happen?
In the meantime, Canadians are living longer and their health care needs are increasing. The big question is: Are we ever going to have enough doctors, nurses and other health care professionals to provide appropriate care to those who need it?
***********************************************
Is your doctor following his own advice?
Yes, says a report in the Medical Post. At least, the majority of them are taking actions to stay healthy.
A Harvard Medical School study says most doctors make an effort to eat wisely and many make a point of working out regularly. Here are some of the findings of a survey of 15,000 physicians:
-82 per cent eat breakfast regularly and consume at least three servings of fruit or vegetables
-only 12 per cent admitted to eating fast food
-nearly 60 per cent chose olive oil over less healthy fats
-about 50 per cent drink alcohol in moderation (fewer than five drinks a week)
– 78 per cent take vitamin supplements regularly
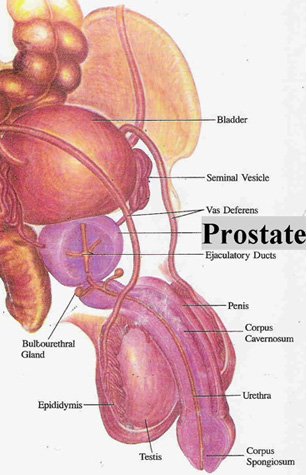
-doctors older than 50, 75 per cent said they had under gone colonoscopy and 84 per cent had PSA test done
-two-thirds of the women older than 40 have had annual mammogram
-majority of the physicians exercised minimum of three times a week
Looks like the majority of the doctors practise what they preach.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!