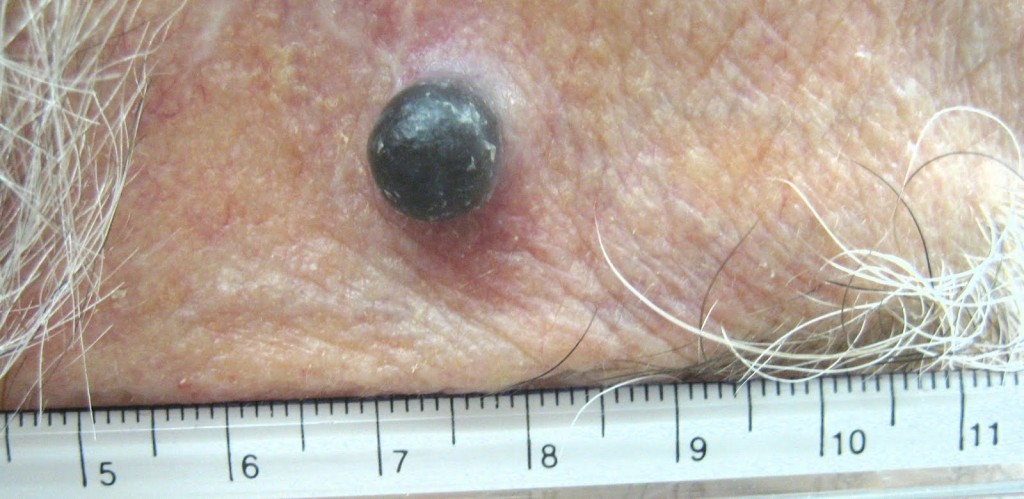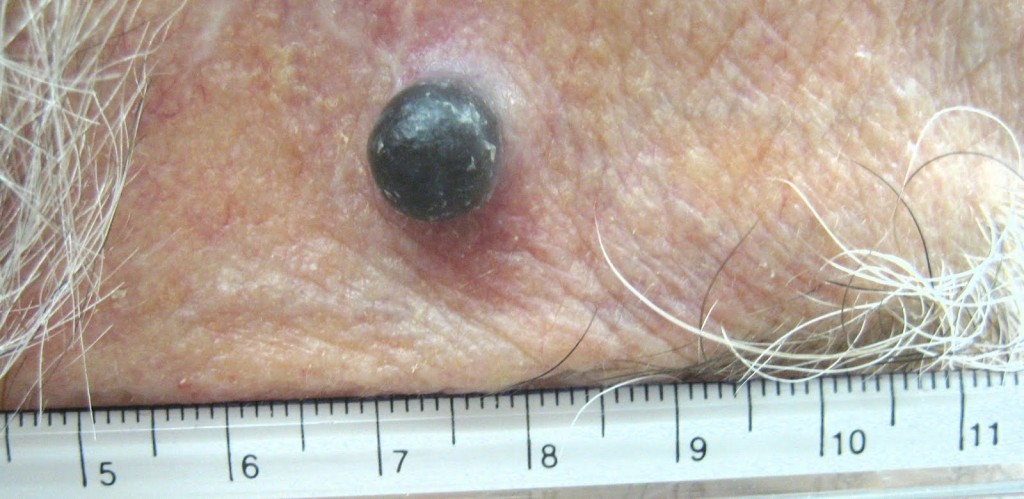
A case of recurrent melanoma in a Caucasian male – temple area.
I enjoy Bob Marley music. I listen to his songs quite often. As most of you know, Bob Marley was a Jamaican singer-songwriter and musician. In May 1981, he died at a very young age of 36 from melanoma. This was tragic. If he would have listened to his doctors then, who knows, he would still be around entertaining us with live performances.
In 1977, Marley was found to have malignant melanoma under the nail of one of his toes. Marley turned down doctors’ advice to have his toe amputated, citing his religious beliefs. He followed the Rastafari tradition. The spread of melanoma to his lungs and brain caused his death. Before his death, he is reported to have said, “Money can’t buy life”.
Bob Marley’s case is interesting from a medical point of view. First, melanoma is not that common in black population and secondly, melanoma under the nail (subungual) is not common either. It is an accepted fact that malignant melanoma in black population and other minority ethnic populations represents an aggressive disease highly associated with invasive lesions. They present with more advanced stage of disease at diagnosis, and consequently with a decreased survival compared with Caucasians.
Melanoma is the sixth most common cancer in North America and the single most common one among young adults 25-29 years old. Lifetime risk of developing melanoma in whites is currently estimated at 1 in 50, compared to 1 in 1000 in African-Americans.
Darker-pigmented populations are consistently reported to have lower risk for melanoma, possibly related to protection from ultraviolet radiation (UVR) provided by melanin.
Melanin is the primary determinant of skin color. It is also found in hair, the pigmented tissue underlying the iris of the eye, and other pigmented areas of the body and brain. The melanin in the skin is produced by cells called melanocytes. Some individuals have very little or no melanin in their bodies, a condition known as albinism.
Production of melanin is stimulated by DNA damage induced by UVB-radiation, and it leads to a delayed development of a tan. It is an excellent photoprotectant. This is because it efficiently absorbs harmful UV-radiation (ultraviolet) and transforms the energy into harmless heat. This prevents the indirect DNA damage that is responsible for the formation of malignant melanoma and other skin cancers.
Caucasians have a predilection to develop lesions on sun-exposed surfaces, including face and neck. Blacks have lesions predominantly located on sun-protected mucosal and acral sites.
Acral sites are the palms, soles, under the nails and in the mouth. It occurs on non hair-bearing surfaces of the body which may or may not be exposed to sunlight. Unlike other forms of melanoma, acral lentiginous melanoma (ALM) does not appear to be linked to sun exposure.
Lentiginous means small, flat, pigmented spot on the skin or under the nail. The reason these lesions have poor prognosis is because they are quite often clinically misdiagnosed.
In fact, an estimated one-third to one-half of all cases of ALM are incorrectly diagnosed at initial presentation as the more commonly appearing benign skin lesions including warts, infections, ulcers, callus, traumatic wounds, and blood clots. Some melanomas have no pigment and these are hard to diagnose early unless you notice some change.
The moral of today’s story is: be vigilant, protect against UV rays, and report to your doctor if there is any change in a mole. If you have a pigmented lesion under a nail, palm of your hands, or sole of your feet which does not go away (a blood clot will slowly disappear) then get a biopsy done. And listen to your doctor. Melanoma can be cured if picked up early.
Long live Bob Marley and his music.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!