During World War II, soldiers lost many man hours due to “jeep disease”. Poor personal hygienic conditions plus the trauma of sitting on hard seats of jeeps driving over difficult terrain were the main reasons why these soldiers suffered from “jeep disease”. But most people who have this condition have never been in the army or driven a jeep.
So, what is “jeep disease”?
Medical name for “jeep disease” is pilonidal disease. It is a spectrum of three conditions: acute pilonidal abscess, chronic pilonidal abscess or sinus, and the unhealed pilonidal surgical wound.
The pilonidal disease most commonly occurs between the buttocks, close to the tailbone. This condition has been described since 1847. The term pilonidal means “hair-nest”. It can also occur in other areas such as beard, the armpit, the belly button and the web spaces of the hands (in barbers) and feet.
For many years, experts believed that this was a congenital condition. In 1946, Patty and Scarff challenged this theory and drew attention to the role of hair in the origin of this problem. Current evidence strongly indicates an acquired origin for pilonidal disease, with most infections being related to penetration of the skin by hair through small midline pits.
Where do these pits come from? Some people believe they are congenital while others believe them to be enlargement of hair follicles. These pits have sinus openings through which the hairs penetrate. Hirsutism in the buttock and perineal area appears to be associated with the development of pilonidal disease.
Management of the condition depends on the type of presentation.
Acute pilonidal abscess needs to be drained immediately once the diagnosis is made. The area should be kept shaved. Daily bath or shower will keep the area clean. Once healed, it may become necessary to excise the midline pits under local or general anaesthesia to prevent recurrence.
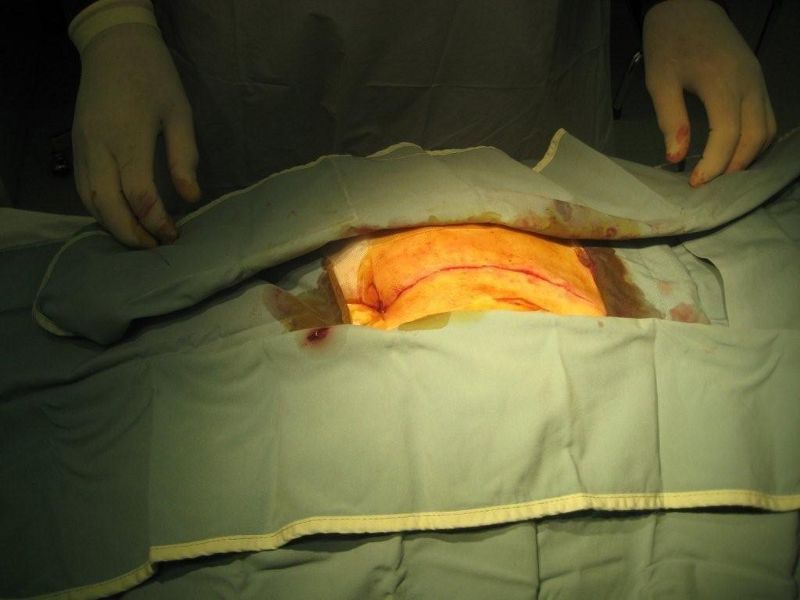
Chronic pilonidal abscess or sinus – treatment of this condition remains controversial as no one treatment has proved superior. The choices are: non-operative treatment with repeated phenol injections; conservative excision of the sinus openings and midline pits; laying open the sinus tract and stitch the skin margins to fibrous tissue (marsupialization); or wide excision with or without different types of closures of the skin.
At medical conferences, I have listened to many experts of the subject and have found no consensus or strong evidence that one treatment is superior to other. Last year, in October, I was in Washington, D.C. attending the American College of Surgeons annual conference. At a luncheon “Meet the Professor” meeting, the subject of pilonidal disease was discussed in great detail. The consensus was that the treatment for this condition should be individualized to each patient according to the severity of the problem.
The unhealed pilonidal surgical wound and recurrence of pilonidal disease after initial treatment is very common. Management of this problem can be very difficult. To start with, the unhealed wound should be curettaged to control the excessive granulation tissue (healing tissue which fills the wound), and the surrounding skin should be shaved weekly. The wound should be kept clean and dry with gauze. Strapping the buttocks apart may help prevent the continuous shearing movement during walking.
The wound may take six to eight weeks to heal. Quite often healing does not occur. Then a skin graft or some form of plastic flap may help the healing process. Overall, treating pilonidal disease should not be taken lightly.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!