Let us start with the word “dyspepsia.” Dyspepsia is a Greek word that means bad or difficult digestion. Some people use the word dyspepsia to mean heartburn.
When a patient says to me, “Doctor, I have dyspepsia or indigestion” then I have to ask more questions. I need to know exactly what the symptoms are. There may be chronic or recurrent pain in the upper abdomen. There may be upper abdominal fullness and feeling full earlier than expected when eating. There may be bloating, belching, nausea, or heartburn.
There is a condition called functional dyspepsia or it used to be called non-ulcer dyspepsia. That means symptoms of dyspepsia are there but there is no pathological finding to account for that. Functional dyspepsia is estimated to affect about 15 per cent of the general population in western countries.
I found an interesting short article in the Canadian Medical Association Journal (CMAJ March 3, 2015) by Sadowski and van Zanten titled “Dyspepsia.”
If the person has alarm symptoms like vomiting, bleeding or anemia, abdominal mass or unintended weight loss, and difficulty swallowing food then he should be referred for an urgent endoscopy of the esophagus, stomach and duodenum.
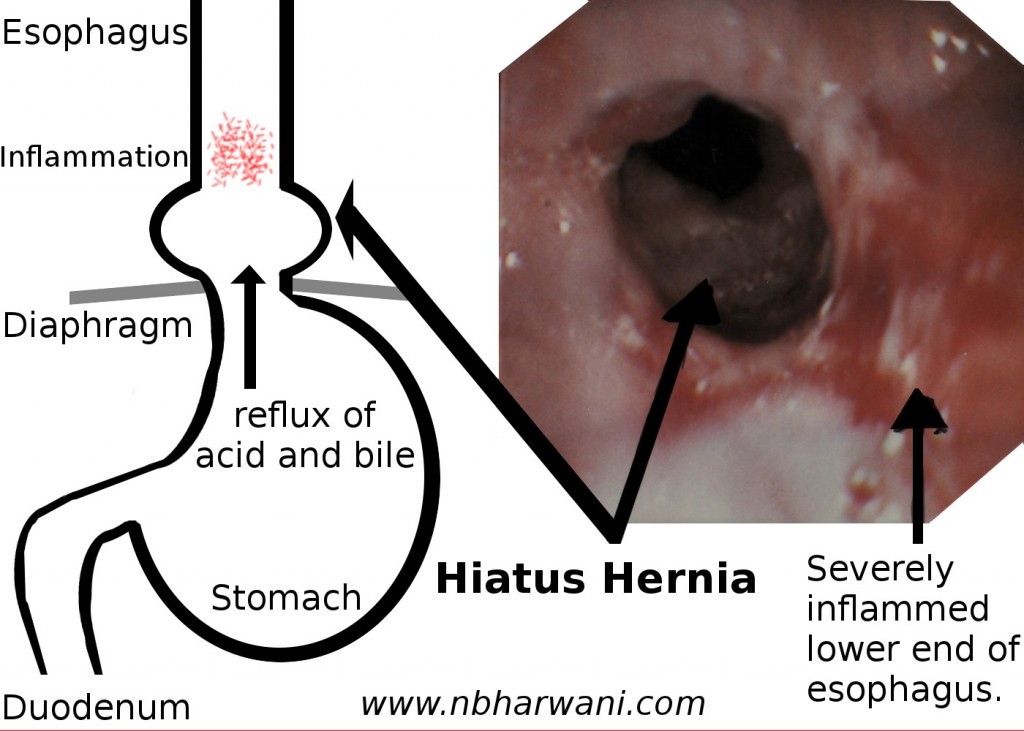
Endoscopy is the preferred diagnostic modality if alarm symptoms are present. If a person with dyspepsia undergoes endoscopy, the most common endoscopic findings for new cases are reflux esophagitis (40 per cent), and gastric and duodenal ulcers (10 percent). No time should be wasted doing barium studies. Doctors should avoid performing an endoscopy for dyspepsia without alarm symptoms for patients under the age of 55 years.
Patients with alarm symptoms who undergo gastroscopy will have clinically significant peptic ulcer disease in 13 per cent of cases and gastric cancer in four per cent of cases. Because the prevalence of serious abnormalities increases with age, an endoscopy should be considered for those aged 55 years or older with new-onset symptoms.
Upper gastrointestinal barium studies are less accurate than endoscopy and should not be used if alarm symptoms are present.
Patients should not be maintained on long-term PPI (proton pump inhibitors used for treating reflux and peptic ulcers) therapy without an attempt to stop or reduce PPI at least once per year in most patients. Examples of PPI are – Losec, Prevacid and Nexium.
Up to 30 per cent of patients with dyspepsia in a Canadian population were found to be taking non-steroidal anti-inflammatory drugs (NSAIDS) including acetylsalicylic acid (Aspirin). Eliminating the use of NSAIDS or dose reduction is often effective for dyspepsia.
The article suggests that an eight-week trial of once-daily PPI therapy can be considered in patients with reflux-like dyspepsia. Those requiring continuous acid-suppressive therapy for symptom control should use the lowest effective dose and try stopping the treatment at least once per year because of potential adverse effects (e.g. bone fractures and infection with Clostridium difficile) of long-term PPI use. Older adults should use the drugs only for the shortest duration possible.
If your symptoms do not disappear after taking PPI for four to six weeks then PPI should be discontinued and further investigations should be done to rule out serious pathology. Patients with new-onset dyspepsia should be tested for Helicobacter pylori infection. Its prevalence in Canada is about 30 per cent, but declining in younger Canadians.
Finally, take it easy on hurry, worry and curry. That is what one English surgeon advised me many years ago.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!