Generally speaking, nearly half of Canadians will get some kind of cancer during their lifetime, according to Canadian Cancer Statistics 2017. Cancer is the leading cause of death in Canada, responsible for one in four deaths.
Today, we will talk about colon and rectal cancer – also known as colorectal cancer.
1. How common is colorectal cancer in Canada?
Colorectal cancer is one of the most common cancers worldwide and the second-most common cancer in Canada. Both men and women are equally at risk. The cancer is most common among people aged 50 and older but can occur in patients as young as teenagers. The average age at the time of diagnosis for men is 68 and for women is 72.
2. Who is at high risk for colorectal cancer?
Over 75 per cent of colorectal cancers happen to people with no known risk factors, which is why regular screening is so important. There are many risk factors. Most common ones are: previous history of colorectal cancer (CRC) and pre-malignant polyps, family history of CRC, genetic predisposition like Lynch syndrome (also called hereditary non-polyposis colorectal cancer, or HNPCC).
3. Signs and symptoms of colorectal cancer include:
A persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool. Rectal bleeding or blood in your stool. Persistent abdominal discomfort, such as cramps, gas or pain. A feeling that your bowel doesn’t empty completely.
4. Who should be screened for colorectal cancer and how often?
Screening program is meant for individuals who have no bowel symptoms or any risk factors. The idea is to pick up cancer in an early stage.
There are many screening programs for early detection of colorectal cancer. They vary slightly in details. Overall, the summary is as follows:
- Asymptomatic people should be screened with a fecal immunochemical test (FIT) every 2 years.
- Abnormal FIT results should be followed up with colonoscopy.
- People ages 50 to 74 without a family history of colorectal cancer who choose to be screened with flexible sigmoidoscopy should be screened every 10 years.
There are two types of tests to check for blood in the stool – FOBT and FIT.
The FOBT can detect blood from any part of the gastrointestinal (GI) tract, while the FIT is more reliable in cases of bleeding from the lower part of the GI tract. The Canadian Task Force on Preventive Health Care published guidelines in 2016 that state people who do not show symptoms and don’t have a strong family history of colorectal cancer start getting screened at age 50.
Not all patients with positive FOBT will have colorectal cancer. No test is one hundred per cent accurate. Overall, about 12 per cent of patients with a positive FOBT have colorectal cancer. If you do an FOBT every two years, you can reduce your risk of dying from bowel cancer by up to a third.
5. Who needs a screening colonoscopy?
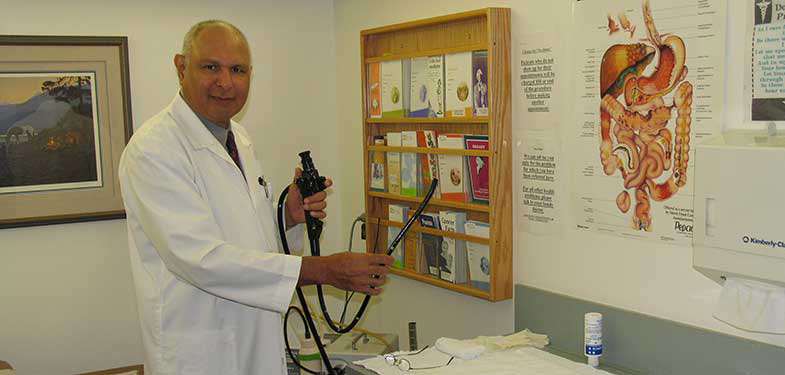
Colonoscopy is considered the gold standard for colon investigation. Indeed, if anything is found on fecal occult blood or by sigmoidoscopy, patients are referred for colonoscopy. It is the test advised for higher risk patients with a family history of colorectal cancer.
New guidelines from the Canadian Association of Gastroenterology urge people with a history of colorectal cancer in their immediate family to start screening earlier and get more frequent checks for the disease. People whose parents, children or siblings have been diagnosed with colorectal cancer are encouraged to get screened between ages 40 and 50, or 10 years earlier than the age at which their relative was diagnosed, whichever comes first.
The whole premise for doing these tests is to pick up pre-malignant polyps and cancer in early stages. Cancer picked up early has 92 per cent five-year survival. If it is in the late stage then the five-year survival is around 10 per cent. Talk to your doctor and get your test done.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!