Almost every household has had a brush with cancer. That means nobody is immune to it. Diagnosis of cancer brings with it tremendous psychological and physical burden to the patient and patient’s loved ones. Therefore, it is important for each one of us to learn something about the common cancers and how to prevent them.
Good news about cancer is that half of all new cancer cases and cancer deaths worldwide are preventable. The second good news is the 5-year relative survival ratio was 62 per cent for all cancers combined from 2001 to 2003. Some years ago it used to be around 50 per cent.
Each year, Canadian Cancer Statistics review the changing size and nature of the cancer burden in Canada. An article in the Canadian Medical Association Journal (CMAJ • November 18, 2008) reviews the major findings from the 2008 edition of Canadian Cancer Statistics.
The article says, “In Canada, cancer will develop in 45 per cent of men and 39 per cent of women during their lifetime, and about one in four Canadians will die of the disease.” There is a higher incidence of cancer among women aged 20-59 years. The mortality rates among women in their 30s and 40s are higher than among men of a comparable age.
Breast cancer is the most prevalent cancer among Canadian women, about one per cent of women. Among men, prostate cancer is the most prevalent cancer, about 0.8 per cent of men.
Thyroid cancer had the highest estimated 5-year relative survival ratio, and pancreatic cancer had the lowest. In general, the incidence rate has been stable for all cancers combined since 1979. In contrast, the mortality rate is decreasing for all cancers combined and for most specific types of cancer. That means we are making slow progress. But we can do more to decrease the incidence of cancer and increase survival if we take more care of our health, take preventative measures and participate in screening protocols.
Breast cancer
The incidence of breast cancer has fluctuated in the last 20 to 30 years due to screening mammography picking up cancer not previously detected. Now the incidence is stabilized to pre-screening years. Good news for women is that in the last 23 years the mortality rate for breast cancer has fallen by more than 25 per cent. Thanks to screening mammography and use of chemotherapy after surgery. Isn’t that wonderful?
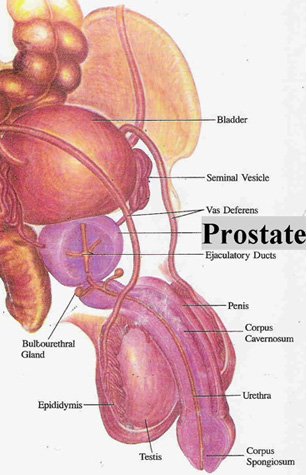
Prostate cancer
The incidence rate of prostate cancer continues to increase moderately. Since the mid-1990s, mortality rates have declined by 2.9 per cent per year, likely because of a combination of earlier detection and improved treatment.
Colorectal cancer
The incidence rate of colorectal cancer, particularly among women, has recently begun to decline. The mortality rate has been falling among both men and women over the past two decades, likely as a result of improvements in chemotherapy.
The article says that screening for colorectal cancer can reduce both the incidence and mortality. Limited screening activity has already been occurring in some provinces, which may account for some of the decline in mortality.
Lung cancer
Among men, the incidence and mortality rates began to decline in the mid-1980s. Among women, incidence and mortality rates have been increasing since at least 1979, and continue to do so (each by 1.2 per cent per year). Overall, the incidence continues to be higher among men than among women. The mortality is also higher among men than among women.
The review shows the 5-year relative survival for cancer has been improving over time. Two of the most common types of cancer, lung and colorectal cancer, the survival rates are poor to fair. Most lung cancers are preventable if you do not smoke. For colorectal cancer, implementation of screening programs in many provinces is expected to improve survival.
Start reading the preview of my book A Doctor's Journey for free on Amazon. Available on Kindle for $2.99!